A 30-year-old lady presents to the emergency division (ED) with headache, nausea, vomiting, diarrhea, and stomach ache that began 1 day in the past. The affected person reviews 3 episodes of nonbilious, nonbloody vomiting with concomitant bilateral extremity weak spot lasting about quarter-hour and a pair of episodes of nonbloody diarrhea.
She reviews intermittent episodes of generalized physique aches and decrease extremity weak spot during the last 2 months. She denies fevers, chills, weight reduction, neck ache, shortness of breath, palpitations, chest ache, or paresthesias.
The affected person has a medical historical past of hypertension for 3 years and sort 2 diabetes for 4 years. She has been noncompliant with drugs for these situations for the final 6 months due to insurance coverage points. It isn’t recognized whether or not she was screened for a secondary reason for hypertension when she initially started remedy.
Her household historical past is noncontributory. She denies smoking in addition to alcohol or drug use. She is a married stay-at-home mother with 2 daughters. She denies a historical past of gestational hypertension or preeclampsia however had a spontaneous abortion at 9 weeks’ gestation inside the final 12 months. The affected person reviews potential latest influenza publicity and is anxious that one thing is incorrect.
Bodily Examination
On arrival, her vitals are as follows: blood stress, 195/126 mm Hg; respiratory fee, 18 breaths per minute unlabored; coronary heart fee, 71 beats per minute; temperature, 98.4 °F; and oxygen saturation, 97% on room air.
On bodily examination, the affected person is somnolent however simply arousable. She is oriented, and her ideas are coherent. She is of common construct with a BMI of 24.8. Her pores and skin is heat and her mucous membranes are moist. She has sweaty palms however no rashes or lesions. Her eyes seem regular with no proptosis. Visible acuity is also regular and extraocular actions are intact.
A small, diffusely enlarged goiter (grade 1 in line with World Well being Group classification) is discovered. A bruit is audible over the goiter however no tenderness or lymphadenopathy is clear. Her lungs are clear to auscultation. Her coronary heart examination reveals clear S1 and S2 with out murmur, rubs, or gallops. Her stomach is flat; no tenderness, plenty, or organomegaly are current. Bowel sounds are normoactive. Pelvic and rectal examinations are regular. Peripheral pulses are intact.
No edema is famous within the decrease extremities. The affected person has full vary of movement, each energetic and passive, of the fingers, wrists, elbows, shoulders, hips, knees, and ankles. Her energy is 5/5 within the higher and decrease extremities bilaterally. Sensations of ache, gentle contact, proprioception, and vibration are intact. All reflexes are 2+.
Laboratory Outcomes
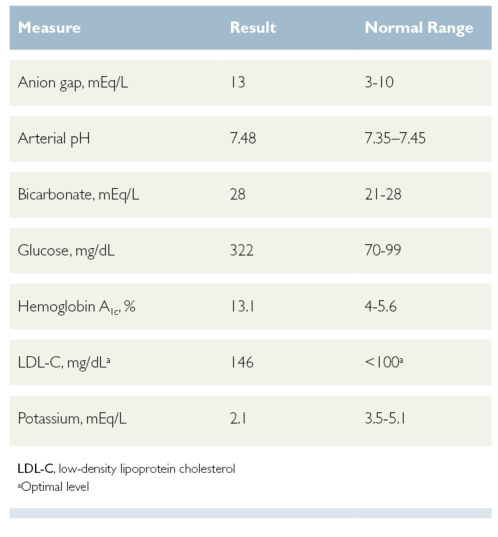
Serum laboratory values are outstanding for a low potassium degree, excessive arterial pH, and borderline excessive bicarbonate degree (Desk). Anion hole, blood glucose, hemoglobin A1c, and low-density lipoprotein levels of cholesterol are elevated. Full blood cell depend, troponin degree, and coagulation research are unremarkable. Serum being pregnant check is adverse.
Desk. Irregular Laboratory Outcomes

The affected person’s electrocardiogram reveals regular sinus rhythm at 71 beats per minute with left axis deviation and T-wave inversion within the inferior lateral leads. Lung fields are clear on chest radiograph.
The affected person is admitted to the cardiology service and instantly is began on labetalol 100 mg orally for elevated blood stress. She reveals little enchancment and standing orders for hydralazine and lisinopril are written. Her blood stress stays elevated; the hydralazine dosage is elevated from 50 to 75 mg and, lastly, to 100 mg 3 occasions a day with the objective of reducing her blood stress to lower than 130/80 mm Hg.
She additionally receives acetaminophen for ache and ondansetron for nausea and/or vomiting as wanted. The affected person refuses prophylactic remedy for influenza publicity however consents to influenza vaccination.
An echocardiogram analysis reveals a left ventricular ejection fraction of 65% (regular vary, 55%-70%); her valves and anatomy are of regular dimension and performance.
An endocrinologist is consulted for her uncontrolled diabetes and goiter. The affected person is began on insulin lispro and insulin glargine. An ultrasound of the thyroid reveals a 1.7-cm nodule on the left lobe and a 5.2-cm nodule on the best. Nevertheless, laboratory analysis of thyroid standing is unremarkable. The affected person’s hypokalemia is handled with 3 doses of potassium chloride powder (40 mEq orally each 4 hours). The affected person’s plasma aldosterone degree is 24.7 ng/dL (regular vary, 1-21 ng/dL) and plasma renin focus is undetectable (regular vary with a traditional sodium eating regimen, 0.6-4.3 ng/mL/h).
Main aldosteronism (PA) is recognized as a possible reason for the affected person’s sickness and a contrast-enhanced computed tomography (CT) of the stomach is ordered to guage for adrenal plenty. The CT reveals a left-sided adrenal mass measuring 2.5 cm × 1.8 cm.
To substantiate the prognosis of PA, a saline infusion check is ordered. In line with PA, the plasma aldosterone focus will increase to 38.7 ng/dL on the 4-hour mark. The affected person’s signs enhance and he or she is discharged on an angiotensin-converting enzyme (ACE) inhibitor for hypertension and a potassium complement.
She receives diabetes dietary training in the course of the hospitalization and insulin coaching. She is discharged on insulin injection and instructed to observe up as scheduled with the endocrine clinic. The affected person is contemplating the advice to biopsy the thyroid nodules. A moderate-intensity statin, (atorvastatin 20 mg each day) is prescribed for hyperlipidemia. She is recommended to observe a low-fat, heart-healthy eating regimen and keep away from being pregnant whereas taking the statin. The affected person has an intrauterine gadget for contraception.
Dialogue
As soon as thought-about a uncommon situation, PA has emerged as a major reason for secondary hypertension, accounting for five% to 10% of sufferers with hypertension and 20% of these with resistant hypertension.1-4 The prevalence of PA is estimated to be 5% to 17%, though this situation is underdiagnosed.1,2
Hyperaldosteronism will be labeled as major or secondary. Secondary hyperaldosteronism is attributable to extreme activation of the renin-angiotensin-aldosterone system (RAAS) attributable to extra-adrenal stimuli, equivalent to a renin-producing tumor, renal artery stenosis, or edematous problems (eg, coronary heart failure, being pregnant).2,4
Main aldosteronism is impartial of the RAAS and is outlined as extreme manufacturing of aldosterone by the adrenal glands.2,4 Extreme manufacturing of aldosterone results in elevated exercise of the sodium-potassium pumps within the cortical accumulating ducts of the nephron, which, in flip, causes sodium retention and potassium loss.4 Hyperaldosteronism additionally causes elevated lack of hydrogen ions in medullary accumulating ducts, leading to metabolic alkalosis.2
Causes of PA embody:
- Aldosterone-producing adrenal adenomas (Conn syndrome): these adenomas sometimes are unilateral however could also be bilateral4
- Adrenal hyperplasia: this can be unilateral or bilateral; hyperplasia is extra widespread amongst older males2,4
- Familial PA: this situation is uncommon and infrequently associated to germline mutations of electrolyte channels2,5
- Ectopic aldosterone-secreting tumors2
- Aldosterone-producing adrenocortical carcinoma2
The most typical scientific manifestation of PA is hypertension that always is immune to remedy.2,5 Hypertension might result in complaints of complications and, if left untreated, might trigger hypertensive retinal modifications, stroke, renal insufficiency, hypertensive encephalopathy, and cardiac failure.6 Regardless of having elevated blood stress, sufferers with PA don’t exhibit peripheral edema.4 Sufferers could also be hypokalemic, even within the absence of potassium-depleting diuretics.4 People who’re severely hypokalemic might current with fatigue, muscle weak spot, ileus, and palpitations.2 Extreme lack of potassium might result in hypokalemia-induced nephrogenic diabetes insipidus, which may trigger polydipsia and/or polyuria.2 Different indicators and signs embody constipation, decreased deep tendon muscle reflexes, and hypomagnesemia.2
Analysis of Main Aldosteronism
The diagnostic strategy to PA begins with routine laboratory research to evaluate serum ranges of sodium, potassium, magnesium, bicarbonate, glucose, blood urea nitrogen, and creatinine. Plasma aldosterone focus (PAC) and plasma aldosterone to renin ratio (ARR) function screening assessments for PA and play an essential position in distinguishing between major and secondary hyperaldosteronism.5 Regular ranges of PAC are lower than 10 ng/dL2; nonetheless, in PA, elevated ranges of plasma aldosterone with decreased or regular renin exercise improve the ratio. An ARR better than 30 ng/dL and PAC better than 20 ng/dL are extremely suspicious for PA, with sensitivity and specificity of better than 90%.2
Confirmatory diagnostic assessments embody a saline infusion check or oral sodium loading.
- Saline infusion check: Affected person is both sitting or mendacity down for at the very least 1 hour earlier than and through a 4-hour infusion of IV regular saline. Plasma ranges for renin, aldosterone, cortisol, and potassium are drawn at hours 0 and 4. Aldosterone ranges of lower than 10 ng/dL after the infusion can rule out the prognosis of PA as a result of ranges don’t lower as they need to in sufferers with PA. Cortisol ranges are taken to exclude adrenocorticotropic hormone isn’t inflicting elevations in aldosterone ranges.2
- Oral sodium loading check: Sufferers ingest 10 g to 12 g of sodium chloride orally for 3 days earlier than testing. On the finish of three days, serum and 24-hour urine are collected and examined for aldosterone, sodium, and potassium ranges. Urine aldosterone ranges better than 14 µg/24 hours are confirmatory for PA. Urine sodium ranges are examined to make sure enough salt loading for correct interpretation of the check.2
To tell apart between causes of PA, thin-sliced adrenal CT with distinction is the most typical preliminary diagnostic check to determine aldosteronomas and adrenal cell carcinoma.5 Ranges of aldosterone in adrenal venous blood could also be measured in sufferers in whom there’s excessive suspicion of unilateral PA regardless of regular imaging.5
Therapy of Main Aldosteronism
The general remedy objective in PA is to scale back the morbidity and mortality related to hypertension, hypokalemia, and different related signs.5 The strategy to remedy depends upon the etiology of the PA. For unilateral adrenal adenomas or adrenal hyperplasia, surgical resection typically is healing.5
Sufferers identified with bilateral adrenal hyperplasia and familial PA require a medical strategy. They need to be began on an aldosterone antagonist equivalent to spironolactone or eplerenone.5 For sufferers with persistent hypertension, clinicians ought to provoke one other antihypertensive agent, equivalent to hydrochlorothiazide or an ACE inhibitor. As well as, they need to advise sufferers to observe a low-salt eating regimen.6
Early prognosis and remedy of PA can enhance a affected person’s general long-term morbidity and mortality. Sufferers with PA have a better danger of creating power kidney illness than people with important hypertension. Nevertheless, when surgical adrenalectomy is carried out, there isn’t any distinction in kidney morbidity.7 Sufferers with PA even have an elevated danger for stroke, atrial fibrillation, coronary heart failure, coronary artery illness, diabetes, and metabolic syndrome than sufferers with important hypertension.8
Conclusion
Main aldosteronism needs to be thought-about in any affected person with treatment-resistant hypertension, particularly in a hypokalemic affected person who isn’t taking a diuretic. Hypertension, unexplained hypokalemia, and metabolic alkalosis are the most typical findings. The workup contains serum electrolytes (to guage for hypokalemia, metabolic alkalosis, hypernatremia, and hypomagnesemia), ARR screening, in addition to a saline infusion or oral sodium loading check and adrenal CT with distinction. People with PA have elevated long-term cardiovascular and renal dangers, making early prognosis and remedy important.
Corinne I. Alois, MS, PA-C, is an assistant professor at St. John’s College Doctor Assistant Program in Jamaica, New York; Alyssa C. Quinlan, PA-C, MPAS, is an assistant professor at St. John’s College Doctor Assistant Program.
References
- Monticone S, Burrello J, Tizzani D, et al. Prevalence and scientific manifestations of major aldosteronism encountered in major care observe. J Am Coll Cardiol. 2017;69(14):1811-1820. doi:10.1016/j.jacc.2017.01.052
- Dominguez A, Muppidi V, Gupta S. Hyperaldosteronism. In: StatPearls. StatPearls Publishing; 2021. Up to date November 21, 2020. Accessed June 22, 2021. https://www.ncbi.nlm.nih.gov/books/NBK499983
- Brown JM, Siddiqui M, Calhoun DA, et al. The unrecognized prevalence of major aldosteronism: a cross-sectional examine. Ann Intern Med. 2020;173(1):10-20. doi:10.7326/M20-0065
- Grossman AB. Main aldosteronism (Conn syndrome). In: Merck Guide Skilled Model. Merck & Co, Inc; 2020. Up to date September 2020. Accessed June 22, 2021. https://www.merckmanuals.com/skilled/endocrine-and-metabolic-disorders/adrenal-disorders/primary-aldosteronism
- Funder JW, Carey RM, Mantero F, et al. The administration of major aldosteronism: case detection, prognosis, and remedy: an Endocrine Society scientific observe guideline. J Clin Endocrinol Metab. 2016;101(5):1889-1916. doi:10.1210/jc.2015-4061
- Iqbal AM, Jamal SF. Important hypertension. In: StatPearls. StatPearls Publishing; 2021. Up to date July 10, 2020. Accessed June 22, 2021. https://www.ncbi.nlm.nih.gov/books/NBK539859/
- Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Renal outcomes in medically and surgically handled major aldosteronism. Hypertension. 2018;72(3):658-666. doi:10.1161/HYPERTENSIONAHA.118.11568
- Monticone S, D’Ascenzo F, Moretti C, et al. Cardiovascular occasions and goal organ harm in major aldosteronism in contrast with important hypertension: a scientific evaluate and meta-analysis. Lancet Diabetes Endocrinol. 2018;6(1):41-50. doi:10.1016/S2213-8587(17)30319-4
This text initially appeared on Scientific Advisor